A case of a 63 yr old male with decreased urine output and sob
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings investigations and come up with diagnosis and treatment plan.
A 63 yr old male resident of Ramanpeta a retired accountant came to the OPD with
CHIEF COMPLAINTS:
decreased urine output since 1 day
Shortness of breath since 1 day
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 1day ago when he developed decreased urine output which was sudden in onset, associated with urgency and pain.
He has shortness of breath since 1 day which is sudden in onset gradually progressive aggravated on walking and relieved by taking rest.
History of abdominal distention and facial puffiness on and off since 3 months.
No history of fever, chest pain, palpitations, cough and cold.
PAST HISTORY:
Known case of hypertension since 2 years
Known case of CAD 2 years back
Known case of hypothyroidism since 1 yr
Not a known case of diabetes mellitus, epilepsy, asthma .
TREATMENT HISTORY:
T.Ramipril and metoprolol for hypertension
T. Thyronorm for hypothyroidism
Percutaneous Coronary Intervention stenting was done for CAD.
History of haemorrhoidectomy 8 years back.
PERSONAL HISTORY:
Before illness : mixed diet, normal appetite, adequate sleep, regular bowel and bladder movements and no allergies
After illness : Diet : consuming foods like idly milk, reduced bladder movements, regular bowel movements, no allergies
He consumed alcohol regularly since 30 years and smoked about 2-3 packs per day before PCI stent placement and stopped afterwards.
FAMILY HISTORY : not significant
GENERAL EXAMINATION :
patient was conscious coherent cooperative moderately built moderately nourished.
No pallor, icterus, cyanosis, clubbing and lymphadenopathy.
Vitals : pulse rate : 74 bpm
Respiratory rate : 32 cpm
Temperature : a febrile
Spo2 : 94%
Blood pressure : 90/60 mm hg
SYSTEMIC EXAMINATION:
Cardiovascular system:
-S1,S2 heard .no mumurs.
Respiratory system:
-Position of trachea central.
- Bilateral airway entry present.
-Dyspnea present
- no wheeze.
Abdomen:
-Distended
-No tenderness
-No palpable mass
-Spleen : not palpable
-liver : not palpable.
CNS examination:
Conscious .
no signs of meningeal irritation.
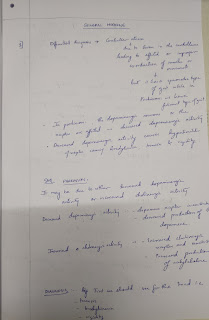
INVESTIGATIONS:
TREATMENT:
Inj. LASIX
Inj. CEFTRIAXONE
Tab. RAMIPRIL 2.5 mg and METOPROLOL 25mg
Tab. ECOSPORIN
Tab.AZITHROMYCIN
Tab. THYRONORM
Nebulization duoline and budecort



Comments
Post a Comment